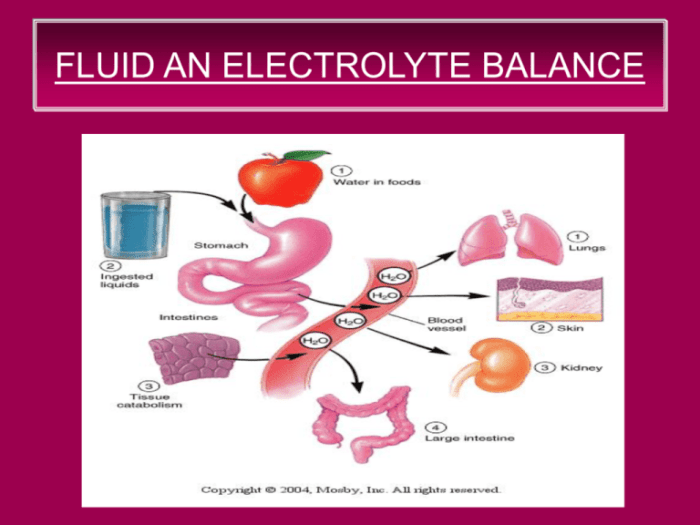
Ati video case study fluid and electrolyte balance heart failure – ATI Video Case Study: Fluid and Electrolyte Balance in Heart Failure delves into the intricate relationship between fluid and electrolyte imbalances in heart failure, providing a comprehensive overview of the pathophysiology, clinical manifestations, assessment, management, and nursing considerations associated with this critical condition.
This case study offers a unique opportunity to explore the complex interplay of impaired cardiac function, neurohormonal activation, and fluid and electrolyte imbalances, shedding light on their profound impact on the clinical presentation and management of heart failure.
Pathophysiology of Heart Failure
Heart failure is a complex clinical syndrome characterized by impaired cardiac function and neurohormonal activation. These alterations lead to a cascade of events that result in fluid and electrolyte imbalances.
Impaired Cardiac Function
Impaired cardiac function, either due to systolic or diastolic dysfunction, leads to a reduction in cardiac output. This decrease in cardiac output triggers a series of compensatory mechanisms, including:
- Activation of the renin-angiotensin-aldosterone system (RAAS)
- Increased sympathetic nervous system activity
- Release of antidiuretic hormone (ADH)
Neurohormonal Activation
The compensatory mechanisms activated in response to impaired cardiac function lead to fluid and electrolyte imbalances. RAAS activation promotes sodium and water retention, while increased sympathetic nervous system activity causes vasoconstriction and further fluid retention.
ADH release promotes water reabsorption in the kidneys, contributing to fluid overload. These hormonal alterations result in increased intravascular volume and interstitial fluid accumulation, leading to edema, dyspnea, and other symptoms of fluid overload.
Clinical Manifestations of Fluid and Electrolyte Imbalances

Fluid and electrolyte imbalances in heart failure can manifest with a range of clinical signs and symptoms.
Fluid Overload
- Edema (peripheral, pulmonary)
- Dyspnea
- Fatigue
- Hepatomegaly
- Ascites
Electrolyte Imbalances, Ati video case study fluid and electrolyte balance heart failure
Electrolyte imbalances can also occur in heart failure and can have significant consequences.
Hyponatremia
Hyponatremia, or low sodium levels, can occur due to excessive fluid retention and dilution of sodium concentration. Symptoms may include:
- Lethargy
- Confusion
- Seizures
- Coma
Hyperkalemia
Hyperkalemia, or high potassium levels, can occur due to impaired renal function and increased potassium release from cells. Symptoms may include:
- Muscle weakness
- Paralysis
- Cardiac arrhythmias
Hypokalemia
Hypokalemia, or low potassium levels, can occur due to diuretic use or excessive sweating. Symptoms may include:
- Muscle weakness
- Fatigue
- Cardiac arrhythmias
Assessment and Diagnosis
Assessment and diagnosis of fluid and electrolyte imbalances in heart failure involve a comprehensive evaluation.
Physical Examination and History Taking
A thorough physical examination and history taking are crucial. Physical signs of fluid overload include edema, jugular venous distension, and pulmonary crackles.
Laboratory Tests
Laboratory tests play a vital role in assessing fluid and electrolyte status. These tests include:
- Serum electrolytes (sodium, potassium, chloride, bicarbonate)
- Brain natriuretic peptide (BNP)
- Creatinine
Imaging Techniques
Imaging techniques can provide valuable information about fluid status and cardiac function.
Echocardiography
Echocardiography can assess left ventricular ejection fraction, valvular function, and pericardial effusion.
Chest X-ray
Chest X-ray can show evidence of pulmonary edema or pleural effusion.
Management of Fluid and Electrolyte Imbalances
Management of fluid and electrolyte imbalances in heart failure aims to improve cardiac function, reduce fluid overload, and correct electrolyte abnormalities.
Diuretics
Diuretics are the mainstay of therapy for fluid overload in heart failure. They promote sodium and water excretion.
| Diuretic Class | Mechanism of Action |
|---|---|
| Loop Diuretics (e.g., furosemide) | Inhibit sodium-potassium-chloride cotransporter in the thick ascending limb of Henle |
| Thiazide Diuretics (e.g., hydrochlorothiazide) | Inhibit sodium-chloride cotransporter in the distal convoluted tubule |
| Potassium-Sparing Diuretics (e.g., spironolactone) | Block aldosterone receptors in the collecting duct |
Electrolyte Supplements
Electrolyte supplements may be necessary to correct electrolyte imbalances.
- Sodium supplements for hyponatremia
- Potassium supplements for hypokalemia
- Calcium supplements for hypocalcemia
Monitoring
Close monitoring of fluid status and electrolyte levels is essential during therapy. This includes:
- Daily weight monitoring
- Regular serum electrolyte measurements
- Assessment of edema and other signs of fluid overload
Nursing Considerations
Nurses play a crucial role in assessing, monitoring, and managing patients with fluid and electrolyte imbalances in heart failure.
Assessment and Monitoring
Nurses are responsible for assessing and monitoring patients for signs and symptoms of fluid overload and electrolyte imbalances.
Interventions
Nursing interventions focus on preventing and managing complications, such as:
- Electrolyte disturbances
- Fluid overload
- Medication administration
Patient Education and Support
Patient education and support are essential for successful management of fluid and electrolyte imbalances.
- Educate patients about their condition and treatment plan
- Provide support and encouragement
- Empower patients to manage their own care
Popular Questions: Ati Video Case Study Fluid And Electrolyte Balance Heart Failure
What is the significance of assessing fluid status in heart failure?
Assessing fluid status is crucial in heart failure as it helps identify fluid overload, a common complication that can exacerbate symptoms and worsen the prognosis. Monitoring fluid status allows healthcare professionals to make informed decisions regarding diuretic therapy and other interventions to manage fluid balance effectively.
How do electrolyte imbalances contribute to the clinical manifestations of heart failure?
Electrolyte imbalances, such as hyponatremia, hyperkalemia, and hypokalemia, can disrupt cardiac function, leading to arrhythmias, muscle weakness, and other complications. These imbalances can further exacerbate the clinical manifestations of heart failure, such as dyspnea, fatigue, and edema.
What is the role of nurses in managing fluid and electrolyte imbalances in heart failure?
Nurses play a pivotal role in assessing and monitoring patients with fluid and electrolyte imbalances in heart failure. They monitor vital signs, observe for signs and symptoms of fluid overload and electrolyte disturbances, and administer medications as prescribed. Nurses also provide patient education and support, empowering patients to manage their condition effectively.